WHAT YOU NEED TO KNOW: What is gastroesophageal reflux in children? Gastroesophageal reflux (GER) occurs when food, liquid, or acid from your child's stomach backs up into his esophagus. What causes gastroesophageal reflux in children? GER often occurs when the lower muscle (sphincter) of your child's esophagus does not close properly. The sphincter normally opens to let food into the stomach. It then closes to keep food and stomach acid in the stomach. If the sphincter does not close properly, food and stomach acid may back up (reflux) into the esophagus. 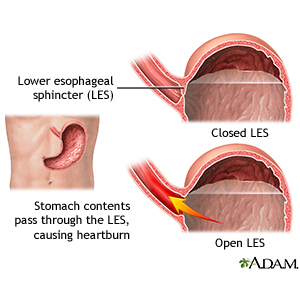
|
The following may also increase your child's risk for GER:- Premature infants: Infants born earlier than expected may have an increased risk for swallowing problems and GER. Infants often outgrow GER by the time they are 12 months old.
- Neurological disorders: Conditions such as cerebral palsy increase your child's risk for GER. Ask your child's healthcare provider for more information about what conditions may lead to GER.
- Asthma: Children who have asthma have a higher risk for GER.
- Specific foods: GER may also occur if your child has an allergy to cow's milk or other foods. Drinks with caffeine may increase your child's risk for GER.
- Smoking: Smoking cigarettes or being around people who smoke often may lead to GER.
What are the signs and symptoms of gastroesophageal reflux? Your child may have no symptoms. If your child has symptoms, he may have one or more of the following: - Breathing problems: Your child may wheeze (make a high-pitched noise) or make a loud, rough noise when he breathes. Some children, mostly infants, may have periods where they stop breathing. This is called an apparent life-threatening event (ALTE). Ask your child's healthcare provider for more information about ALTEs.
- Cough and voice changes: GER may cause your child to cough often. Your child's voice may also change or sound hoarse when he has GER.
- Heartburn: Heartburn is when your child has a painful, burning feeling in his chest. Heartburn often occurs after eating. The burning feeling comes from stomach contents or acid that backs up into his esophagus. Your child may have abdominal pain and trouble sleeping. Your child may also belch often or get the hiccups.
- Irritability: Your child may become fussy and cry often. He may begin crying for no known reason and be hard to calm.
- Poor feeding and growth: With GER, your child may not eat the right amounts of food to help him grow. He may be shorter or weigh less than other children his age. Infants with GER may arch their back when they are fed.
- Swallowing problems: Your child may have problems swallowing food and liquids. He may feel like he has a lump in his throat. Your child may also feel pain when he swallows.
- Regurgitation or vomiting: Regurgitation is the backing up of stomach contents into your child's throat or mouth. Vomiting more commonly occurs in infants. He may vomit without feeling sick first. When your child vomits often, you may see blood in his vomit.
How is gastroesophageal reflux in children diagnosed? Your child's healthcare provider will do a physical exam. He will ask about your child's symptoms and when they started. Tell your child's healthcare provider about your child's medical conditions, eating habits, and activities. Your child's healthcare provider may ask about any family history of GER and if any stressful events have happened lately. If your child has been vomiting, tell his healthcare provider how often and how much he vomits and if he feels pain. Also tell your child's healthcare provider if you have noticed blood in your child's vomit. Your child's healthcare provider may do any of the following tests: - Upper gastrointestinal x-rays: During an upper gastrointestinal (GI) x-ray, pictures are taken of your child's upper GI tract. The upper GI tract includes the esophagus, stomach and intestines (bowel). Your child may be given a chalky liquid to drink before the pictures are taken. This liquid helps your child's stomach and intestines show up better on the x-rays. This test may show if upper GI problems are causing your child's GER.
- Nuclear scintigraphy: During nuclear scintigraphy, a machine is used to take pictures of your child's stomach and esophagus. Your child will be asked to swallow food or a formula that has radioactive liquid in it. This test may show how well his stomach empties and if he has reflux. Your child's healthcare provider may also check if your child is aspirating. Aspirating occurs when liquid or food goes into your child's lungs.
- Endoscopy: An endoscopy uses an endoscope to see the inside of your child's digestive tract. An endoscope is a long flexible tube with a light and camera on the end. During an endoscopy, healthcare providers will look for any tissue damage in your child's esophagus. Healthcare providers will also look for problems with how your child's digestive tract is working. A biopsy (tissue sample) may be taken from your child's digestive tract and sent to a lab for tests.
- Esophageal pH monitoring: During esophageal pH monitoring, the pH (acid or base levels) in your child's esophagus is measured. Sensors are put into your child's nose and down into his esophagus. The sensors will normally be left in place for a day. This test measures how much and how often stomach acid refluxes into your child's esophagus.
How is gastroesophageal reflux in children treated? The goal of treatment is to relieve your child's symptoms and prevent damage to his esophagus. Treatment is also done to promote healthy weight gain and growth. Your child may need the following: - Medicine:
- Histamine type-2 receptor blocker: This group of medicines is also called H2 blockers. They block acid production in your child's stomach.
- Proton pump inhibitor (PPI): This medicine blocks acid from forming in your child's stomach.
- Antacids: This medicine decreases the stomach acid that can irritate your child's esophagus and stomach.
- Prokinetic medicine: Prokinetic medicine decreases the amount of time food stays in your child's stomach. When your child's stomach empties properly, he may have a decreased risk for reflux.
- Surgery: Surgery may be needed if your child's GER does not improve with other treatments. Your child may need surgery to correct a part of his stomach or tighten the lower esophageal sphincter. He may also need a tube placed into his abdomen to decrease the risk for GER. Ask your child's healthcare provider for more information on surgery to help his GER.
What can I do to help my child with GER? - Keep a diary of your child's symptoms: Write down when your child becomes fussy, cries for no reason, or has trouble sleeping. Write down what your child is doing when symptoms occur. Bring the diary to your child's visits with his healthcare provider. The diary may help your child's healthcare provider plan the best treatment for him.
- Feed your infant thickened or special formula: Thickening your infant's milk or formula may decrease how often he vomits. Rice-cereal can be added to your infant's feeding to make it thicker. You may also try to feed your child hypoallergenic milk formula to decrease GER. Smaller feedings more often may also help decrease your infant's GER.
- Position your infant after feedings to decrease his symptoms: After you feed your infant, keep him sitting upright for 90 minutes to decrease GER. Laying your infant on his left side after he eats may also help decrease his risk for reflux.
- Have your child sleep on his left side with his head raised: This may decrease his reflux while he sleeps. The head of your child's bed can be raised by placing pillows or blocks under his mattress.
- Help your child make good food choices: If your child is overweight, his risk for GER increases. Spicy foods, chocolate, and drinks with caffeine should be avoided. Make sure your child knows that staying away from certain foods may help him feel better. Talk to your child's healthcare provider about the best food choices him.
- Keep your child away from cigarette smoke: Do not smoke or allow others to smoke around your child. If your child smokes, help him to stop. Smoking can worsen your child's GER and harm his heart, lungs, and blood.
What are the risks when my child has gastroesophageal reflux? - Your child may have an allergic response to the medicines used to treat his GER. He made need surgery if his symptoms do not improve or become worse. During surgery, your child may bleed more than expected. After surgery, your child may get an infection. Your child's stomach may become swollen or bloated after surgery. His esophagus may swell and make it hard to swallow. He may also be at risk for seizures.
- Without treatment of GER, your child may get ear, nose, throat, and lung infections more often. Stomach acid reflux may damage his vocal cords. Your child may refuse to eat and drink and he may not grow properly. Your child may also become dehydrated (not enough body fluid). When stomach acid backs up into your child's esophagus, it may damage the tissue lining. The lining of his esophagus may swell and make it hard to swallow. Damaged tissue may cause your child to vomit blood. Over time, the damage GER causes in the esophagus may lead to cancer. If your infant has ALTEs, he may have an increased risk for sudden infant death syndrome (SIDS).
When should I contact my child's healthcare provider? - Your child becomes more irritable or fussy and does not want to eat.
- Your child becomes weak and urinates less than normal.
- Your child is losing weight when he should not be.
- Your child has ear pain.
- Your child has more trouble swallowing than he has before, or he feels new pain when he swallows.
- Your infant arches his back during feedings.
- You have questions or concerns about your child's condition or care.
When should I seek immediate care or call 911? - Your child suddenly stops breathing, begins choking, or his body becomes stiff or limp.
- Your child's skin turns blue or very red.
- Your child suddenly has trouble breathing or makes new noises when he breathes.
- Your child vomits more blood than he has before, or he vomits blood for the first time.
- Your child has severe chest pain.
- Your child has severe stomach pain and swelling.
|