WHAT YOU NEED TO KNOW: What is intrathecal (IT) chemotherapy (chemo)? IT chemo is given to kill cancer cells in your cerebrospinal fluid (CSF). CSF is the fluid that surrounds your brain and spinal cord. IT chemo is also given to prevent cancer from spreading to your CSF from other places. What will my chemo schedule be? - How often and how long you get chemo will depend on the type of cancer you have. It will also depend on the type of chemo you need, side effects, and how well the chemo works. You may need IT chemo and another type of chemo, such as intravenous chemo.
- Chemo is often given in cycles over a period of several months or more. This means that you will get the medicine for a period of time, and then you will have a break from it. This allows your body to grow new, healthy cells. You may need more than 1 cycle of chemo to treat your cancer.
How do I prepare for IT chemo? You may need to stop taking blood thinners or NSAIDs several days before IT chemo. This will prevent bleeding in your spine or brain. Have someone drive you home after IT chemo and stay with you for 24 hours. This person can help care for you and call 911 if you have problems. How is IT chemo given through an Ommaya reservoir? An Ommaya reservoir is a small container placed under your scalp during surgery. The reservoir is connected to a small tube that sits inside your brain. Your healthcare provider will insert the needle through your scalp and into the Ommaya reservoir. He will inject the chemo into the reservoir. The chemo will travel throughout your CSF. It will help kill cancer cells in the fluid that surrounds your brain or spine. Your healthcare provider will remove the needle and cover the area with a bandage. 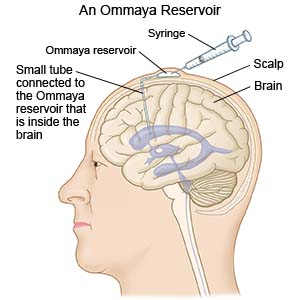
|
How is IT chemo given through a lumbar puncture (LP)? A lumbar puncture is a procedure to inject chemo into your CSF. The injection is usually given in your lower back. Before an LP, your healthcare provider will numb the area. He may also give you IV medicine to help you relax. He will insert a needle into the spaces between your spine (CSF) and inject the chemo. It may take 10 to 30 minutes to finish the injection. When the injection is done, he will remove the needle and cover the area with a bandage. You will need to lie flat for 30 to 60 minutes after the procedure. This will help the chemo travel throughout your CSF and kill cancer cells. It will also help prevent a headache. What are the risks of IT chemo? IT chemo may cause a headache, fever, nausea, or vomiting. It may also cause your eyes to be sensitive to light. Spinal fluid may leak from the LP site. Your nerves or spinal cord may be damaged during an LP. If you have an Ommaya reservoir, it may become twisted or blocked. You may have an allergic reaction to the chemo or get an infection in your spine or brain. IT chemo may cause seizures. This may become life-threatening. What other tests or treatments may I need during chemo? Your healthcare provider may remove samples of CSF through an LP or your Ommaya reservoir. Samples may be removed on the day of chemo. The samples will be sent to the lab and tested for cancer cells. Your healthcare provider may order tests to check how the chemo is working. Tests will also check for problems that chemo may cause. CT or MRI pictures of your brain or spine will show if your tumor has shrunk. These tests will also show if cancer has spread to other places in your body. What can I do to care for myself after I get IT chemo? - Care for the injection site as directed. Ask your healthcare provider when you can remove the bandage. Also ask when the site can get wet. Let soap and water gently run over the site. Do not scrub. Pat the area dry and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. Do not put powders or lotions on the area unless your healthcare provider says it is okay. Use a clean towel or washcloth to put firm, steady, pressure on the site if it bleeds. You may need to hold pressure for 5 to 10 minutes to stop the bleeding.
- Rest as needed. Lie flat for 30 minutes if you get a headache after treatment. You may feel tired for a few days after getting chemo. Return to activities slowly, and do more as you feel stronger.
- Drink plenty of liquids. This will help prevent a headache after IT chemo. Ask how much liquid to drink each day and which liquids are best for you.
- Prevent infection. Stay away from people who are sick. Wash your hands frequently and ask visitors to wash their hands. Ask family and friends not to visit if they are sick. Do not spend time in crowded places such as movie theaters, malls, or elevators. Ask your healthcare provider if you need vaccines.
Where can I find more information and support? It may be difficult for you and your family to go through cancer and cancer treatments. Join a support group or talk with others who have gone through treatment. - American Cancer Society
250 Williams Street
Atlanta , GA 30303
Phone: 1- 800 - 227-2345
Web Address: http://www.cancer.org
- National Cancer Institute
6116 Executive Boulevard, Suite 300
Bethesda , MD 20892-8322
Phone: 1- 800 - 422-6237
Web Address: http://www.cancer.gov
Call 911 or have someone else call for any of the following: - You have chest pain, shortness of breath, or trouble breathing.
- Your throat feels swollen and you have trouble swallowing or breathing.
- You have a seizure.
- You cannot be woken.
When should I seek immediate care? - You feel confused.
- You have a severe headache and a stiff neck.
- You have vision or hearing loss.
- You have arm or leg weakness or trouble walking.
- You urinate a lot less than usual or stop urinating.
- You feel weak, dizzy, or faint.
- Your heart is beating faster than usual.
- You cannot stop bleeding from your injection site after you hold pressure for 10 minutes.
- You have clear fluid leaking from your injection site.
When should I contact my oncologist? - You have a fever of 100.5° F or higher or chills.
- You have nausea or are vomiting.
- You feel depressed.
- You have questions or concerns about your condition or care.
|